Medical Billing and Coding Changes in 2021
 July 30, 2021
July 30, 2021Every year comes with change.
The content of the Current Procedural Terminology (CPT) coding manual is no exception. The American Medical Association consistently adds, erases, or reexamines codes/descriptors. Often, we are the ones who expect and monitor these changes since we need to update coding, billing, and documentation rules. In the new version, doctors practicing anesthesia and pain management will have less burden to bear. The guide also provides information on documentation, utilization, and coding from the 2021 CPT manual.
- Code Changes in CPT Manual 2021
The CPT code changes are the most important announcement in the CPT code manual. Here are a few of them:
- Transforaminal Injections under ultrasound guidance were deleted from the Pain Management section (CPT codes 0228T- 0231T), and are now reported by the unlisted code 64999.
- The CPT code changes for 2021 involved codes found in the Surgery Section, Pathology/ Laboratory Section, and Category III Section of the CPT manual. The CPT code for High Intensity Focused Ultrasound (HIFU) — ablation of malignant prostate tissue is 55880. However, carrier policies are still reporting this process to be a trial and need approval before reimbursement begins. The FDA thus approves the CPT code, so any updates in reimbursement status will be reviewed.
- The 2021 CPT edition contains 206 new codes, 69 revised codes, and 54 omitted codes.
This change is meant to bring the process up to date with current standards. According to AMA, it highlights the increase of certain medical conditions that were minor before together with other codes.
- Changes in E/M 2021 Coding Guidelines
The Evaluation and Management (E/M) 2021 coding guidelines related to Office Outpatient visits (CPT 99202-99215) have changed. Here are some of them:
- CPT 99201 is not anymore in the CPT code manual.
- Providing guidance is necessary for medical decision-making about latent illnesses and comorbidities.
- Physical exams and history are not necessary for code selection.
- It is necessary to add details in coding guidelines and descriptions to promote payer consistency.
- Medical decision-making (MDM) levels or total time spent on each date dictate the code selection for 99202-99205, which includes “a medically appropriate history and/or physical examination.”
- Office/Outpatient 2021 E/M Codes — New Patient
Furthermore, the 2021 coding guidelines 99202-99205 follow the same structure as 99203 example below:
- 99203 – Office and Outpatient visits for E/M of new patient coding guidelines require “a medically appropriate history and/or examination” and low level of MDM. A total time of 30-44 minutes is spent on the date of the encounter for code selection.
| Code | History/Exam | MDM | Total Minutes |
| 99202 | Medically appropriate history and/or examination | Straightforward | 15-29 |
| 99203 | Medically appropriate history and/or examination | Low | 30-44 |
| 99204 | Medically appropriate history and/or examination | Moderate | 45-59 |
| 99205 | Medically appropriate history and/or examination | High | 60-74 |
Additionally, the CPT code +99417 was created by AMA for prolonged E/M services longer than 74 minutes of the primary procedure. This code would be used as follows:
| Code/s | Total Duration of New Patient Office/Outpatient Services (with the use of code 99205) |
| No separate report | < 75 minutes |
| 99201 X 1 and 99417 X 1 | 75 – 89 minutes |
| 99205 X 1 and 99417 X 2 | 90 – 104 minutes |
| 99205 X 1 and 99417 X 3 or more for additional (15 minutes each) | 105 minutes or greater than |
- Office/Outpatient 2021 E/M Codes — Established Patient
New patient codes and established patient codes require different times for each level. The illustration below states level 5 established-patient code 99215 lists 40-54 minutes while level-5 new-patient code 99205 lists 60-74 minutes.
| Code | History/Exam | MDM | Total Minutes |
| 99212 | Medical appropriate history and/or examination | Straightforward | 10-19 |
| 99213 | Medical appropriate history and/or examination | Low | 20-29 |
| 99214 | Medical appropriate history and/or examination | Moderate | 30-39 |
| 99215 | Medical appropriate history and/or examination | High | 40-54 |
Therefore, payers who follow AMA can now use the new prolonged services code +99417. For services 55 minutes or longer, this code can be an add-on.
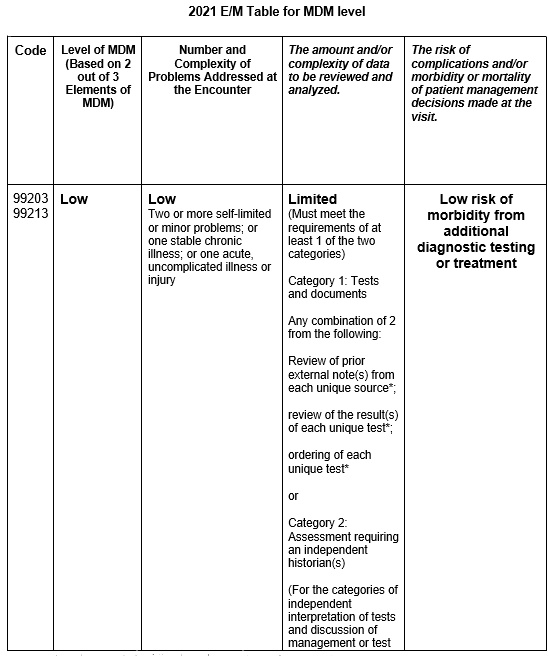
- 2021 E/M Guidelines for MDM
The CPT proclaims that MDM “includes diagnosing, assessing conditions, and selecting appropriate management options.” In 2021, three components characterize MDM for office/outpatient visits. These components are comparable, however not the same as those of 2020:
- The number and complexity of the problem or problems the provider addresses during the E/M encounter.
They will address the problem after the evaluation and treatment at the encounter physician or other qualified professional.
- The amount and/or complexity of data to be reviewed and analyzed.
The 2021 guidelines list divided the data into three:
- Tests, documents, orders, or independent historians
- Independent interpretation of tests
- Discussion management with external physicians/appropriate sources
- The risk of complications and/or morbidity or mortality of patient management decisions made at the visit.
In the 2021 guidelines, options still need consideration but not for selection. They are still taken into account after the patient and family hear about the MDM. Some examples can be:
- Deciding whether to hospitalize a psychiatric patient with adequate support for outpatient treatment.
- Decide palliative care for a patient with advanced dementia and acute condition of sickness.
The basis for meeting requirements for two out of three elements is also at the level of the MDM column. Notably, physicians should be familiar with the column for Amount and/or Complexity of Data to be Reviewed and Analyzed. Indeed, the categories on it are essential for understanding the structure.
In the table, codes 99203 and 99213 need to meet the criteria for at least one of two categories. For codes 99204 and 99214, the service has to meet the requirements for one of three categories. For the highest-level codes, 99205 and 99215, the service needs to meet the requirements for two of three categories. Lower-level codes don’t have categories in that column.
- Codes link to Technology Development.
There is more consideration to these progressions when it comes to advanced technology. Medical billing guidelines and code changes are gradually improving quality treatment in the health care system. Rather than coordinating with codes to new methods, doctors and medical billing clinical staff now have efficient documentation services for patients. In addition, there is increasing recognition that not all patient care occurs in the doctor’s office. As part of the new coding guidelines, some tasks also happen at other times, such as coordination of care or telehealth visits.
These 2021 coding guidelines will also help progress documentation to inpatient care, though there may be hurdles and pins. Also, you can inquire for assistance from medical billing experts. They are willing to help shape up these changes and make your medical practice foster.
Tap Into Our Expertise
At 5 Star Billing Billing Services Inc, we offer the highest level of performance for high-quality medical billing and coding. Save your money by outsourcing to a professional billing service.


1 Comment
I do agree that coding guidelines can help a medical practice’s billing system improve the efficiency of its documentation services. I would imagine the difficulty in managing without the aid of technology. That’s why, getting a good system, is crucial for medical services to have significant growth.