2023 CMS Pain Management Codes
 April 5, 2023
April 5, 2023Chronic pain affects more than 50.2 million Americans, making the CPM bundled payment an essential and timely intervention. With this payment, patients can benefit from a comprehensive, person-centered plan of care that includes diagnosis, care coordination, medication management, and other elements of integrated, multimodal pain care.
The Centers for Medicare & Medicaid Services (CMS) continuously strives to give more people access to evidence-based treatments for acute and chronic pain and enhance the care experience for people with pain.
We’ll discuss the 2023 CMS Pain Management Codes list with you in this article.
The Centers for Medicare & Medicaid Services (CMS) Pain Management Codes for 2023
The start of a new year is exciting. However, you must know the latest CMS CPT codes as a pain management provider. That is why the CMS rolled out new chronic pain management codes, including bundled care, evaluation and management, telecare visits, and more.
With the release of the 2023 Medicare Physician Fee Schedule Final Rule on November 18, 2022, providers can learn about the code changes and how to report them properly for reimbursement.
Stay current on the latest CMS CPT codes for your pain management practice to ensure you receive the proper reimbursement.
New CMS Codes for “Bundled” Care
As a pain management provider, you don’t have to worry about billing or coding services separately. You can now use the 2023 CMS chronic care management codes to report on the monthly care you provide. This process makes billing for these services easier since specialists can now report the bundled code monthly. To make sure you have an understanding of what is included in the Chronic Pain Management coding (CPM) bundle, be sure to review the code descriptor.
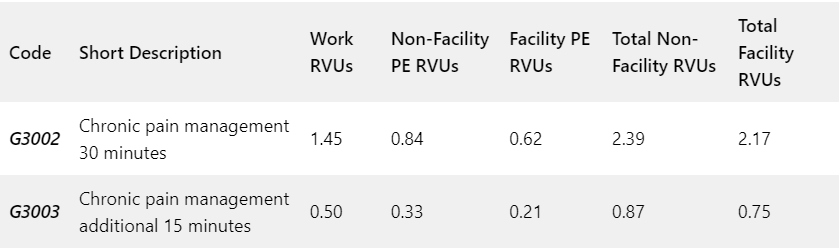
Code Descriptors for the New Chronic Pain Management CPT Codes
| HCPCS Code G3002 | Chronic pain management and treatment, monthly bundle including, diagnosis; assessment and monitoring; administration of a validated pain rating scale or tool; the development, implementation, revision, and/or maintenance of a person-centered care plan that includes strengths, goals, clinical needs, and desired outcomes; overall treatment management; facilitation and coordination of any necessary behavioral health treatment; medication management; pain and health literacy counseling; any necessary chronic pain related crisis care; and ongoing communication and care coordination between relevant practitioners furnishing e.g. physical therapy and occupational therapy, complementary and integrative approaches, and community-based care, as appropriate. Required initial face-to-face visit at least 30 minutes provided by a physician or other qualified health professional; first 30 minutes personally provided by physician or other qualified healthcare professional, per calendar month. (When using G3002, 30 minutes must be met or exceeded.) |
| HCPCS Code G3003 | Each additional 15 minutes of chronic pain management and treatment by a physician or other qualified healthcare professional, per calendar month (List separately in addition to code for G3002). (When using G3003, 15 minutes must be met or exceeded.) |
The HCPCS code G3002 describes assessing, diagnosing, and monitoring a patient’s pain, combined with their treatment and coordination with other clinicians.
Take Note: This HCPCS code only describes the first 30 minutes of chronic pain management services.
If you spend over 30 minutes on CPM with the patient, you can report the new add-on code G3003.
Definition of Chronic Pain
Physicians have long encountered difficulties providing evidence to Medicare payers for “chronic” conditions because the agency does not specify its interpretation. Currently, CMS defines chronic pain as “persistent or recurrent discomfort lasting more than three months.” Despite this definition, some providers may believe CPM codes cover only existing patients.
The Fee Schedule states specifically:
The beneficiary, at the first visit, need not have an established history or diagnosis of chronic pain or be diagnosed with the condition that causes or involves chronic pain; rather, it is the clinician’s responsibility to establish, confirm, or reject a chronic pain and/or pain-related diagnosis when the beneficiary first presents for care and the clinician is using HCPCS code G3002.
CMS 2023 E/M Changes
It is now possible to report evaluation and management (E/M) visits (99202-99215 in the office setting) along with CPM codes as long as the documentation indicates that an E/M visit was performed separately from the time documented for the CPM visit. Anyone who reviews the patient records should be able to identify the E/M documentation from the CPM note. Moreover, both should stand on their own regarding the time spent and the information covered.
- Updates on Telehealth
CMS has added CPM to its list of telehealth services, with one significant stipulation: the initial visit must be in person. Afterward, the patient can present through telehealth for subsequent visits.
Due to the lifting of COVID-19 regulations, telehealth regulations may change in the near future. Keeping track of any extensions to the PHE expiration date is also necessary.
If you’re looking for additional information, please check out the CMS Website.
CMS Additional Regulations and Requirements for Billing the Chronic Pain Management Codes.
The billing for pain management codes must match the service described in the code descriptors. Check out the additional CMS guidelines for 2023 below:
- Auxiliary personnel may not provide services incident to a physician’s (or other QHP) professional duties.
- During the initial visit, the beneficiary must provide verbal consent, and it must be recorded in the beneficiary’s medical records. There is a need to educate beneficiaries on what CPM stands for, how often they may expect to receive the services, and what cost-sharing may be relevant to their circumstances.
- CPM services may be billed on the same date as E/M services. Moreover, these services can be billed in the same month as remote physiologic monitoring (RPM) services, remote therapeutic monitoring (RTM) services, and care management services (such as chronic care management (CCM), transitional care management (TCM), or behavioral health integration (BHI) services), if all the criteria for reporting each service is fulfilled. Nevertheless, the time spent providing CPM services cannot be counted as time for any other service that has been provided and billed.
- The HCPCS code G3002 may be billed by an unlimited number of physicians for a beneficiary for a month, if medically necessary. G3003 can be billed multiple times for a particular beneficiary and month, if medically necessary, once G3002 has already been billed. Despite this, CMS will monitor utilization.
- The scope of CPM services is limited to outpatient and home care settings.
Summary of Chronic Pain Management Codes
The Centers for Medicare & Medicaid Services (CMS) created a new code set to reimburse providers for treating chronic pain patients. It’s also good that CMS acknowledges the significance of care management services in improving patient outcomes and reducing healthcare costs.
Note: HCPCS codes describe drugs, supplies, and other services not included in CPT codes. Furthermore, CPT and HCPCS codes have 5 characters, but HCPCS begins with a letter, and the rest are numbers. CMS administers HCPCS codes, not the AMA.

