Best Guide to E-Visit Documentation, Coding, and Billing August 3, 2022

The American Academy of Family Physicians (AAFP) encourages safe, secure online interactions between physicians and patients, such as electronic visits or “virtual e-visits.” In non-emergency situations, e-visits can substitute for office visits with primary care providers. It is a fast and easy online procedure for patients to receive a diagnosis and treatment plan.
This article will give you the best guide to e-visit documentation, coding, and billing.
What Should Providers Know About E-visits?
An encounter must meet the following criteria to be considered an e-visit:
- The practice must have a well-established relationship with its patients.
- E-visits require patient consent and a communication request.
- The patient must initiate non-face-to-face electronic communication. For example, patient portal systems.
- Patients must not have seen an office visit to a physician or therapist for the same clinical concern in the past seven days.
- It is only possible to report e-visits every seven days.
- An e-visit is not the same as typical therapy sessions.
For e-visits, the following documentation requirements are needed:
- The main complaint with all evaluation and management services (E/M).
- The specifics of treatments, assessment of diagnoses or symptoms, evaluation, and conversation.
- An official patient consent record is backed up by a signature and captured in the clinical note. Moreover, e-visit software platforms accept scanned copies of signed consents. Some systems allow electronic signatures.
- The total time recorded over the seven days supporting the billable service.
List of Current Procedural Terminology (CPT) Codes That Require Providers to Follow Policies Set by Payers
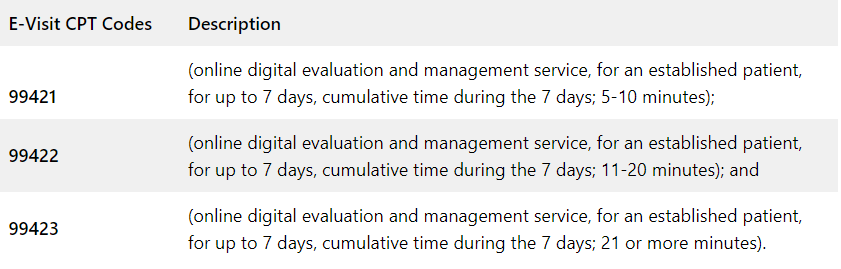
The codes for online digital evaluation services (e-visits) used by doctors are complex. Below are the codes used:
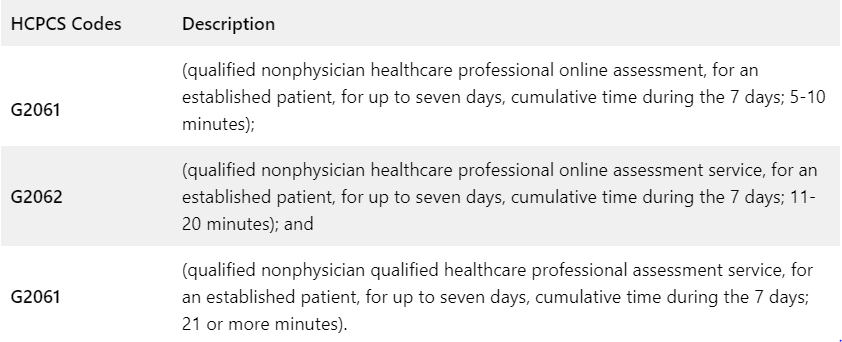
Medicare uses the following HCPCS codes and descriptors for qualified non-physician professionals for its online digital evaluation service (e-visit):
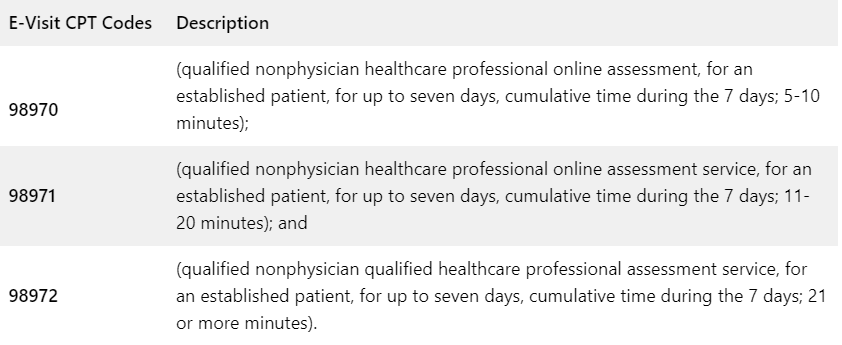
Private payers and workers’ compensation are using the following online digital evaluation service (e-visit) CPT codes and descriptors:
Do’s and Don’ts in Billing E-Visits
When the following conditions are met, you can bill an e-visit:
- The provider establishes a relationship with the patient.
- Response time by the provider is longer than five minutes.
- A provider responds through the patient portal to a message initiated by the patient.
- A visit meets the 2021 E/M guidelines.
- It has been seven days since the clinician last saw the patient.
- There is no global period for the same or similar condition for the patient.
- In this case, the provider is making a clinical decision that would normally be performed in the office (e.g., medication dose adjustment, ordering a test, or prescribing a new medication).
- A patient has consented to the e-visit and understands that he may be billed.
- For online digital E/M services, the service period includes all related work done within seven days by the reporting individual and other registered healthcare providers (RHPs) in the same group practice.
- The 7-day period begins when the reporting provider reviews the patient’s inquiry personally for the first time.
- A new/unrelated problem from the patient arises within seven days of the previous E/M visit for a different issue.
Do not bill an E-visit in the following situations:
- During the 7-day period, the provider may bill for other separately reported services (such as care management, INR monitoring, remote monitoring, etc.)
- The same or similar condition was billed to the patient for an e-visit within the past 7 days.
- The patient inquires about a surgical procedure that happens during the surgery’s postoperative period (global).
- Providers are simply disseminating results, processing medication requests, or scheduling appointments (for billing, E/M services must be performed).
- A separate face-to-face E/M service (either in person or via telehealth) happens (included in the E/M) during the 7-day period of the e-visit.
- Besides clinical staff time, only provider time can be included.
The AAFP published an algorithm in response to the growing number of virtual visits. It was developed by James Dom Dera, MD, FAAFP, to determine which code should be used for virtual services.
Tap Into Our Expertise
At 5 Star Billing Billing Services Inc, we offer the highest level of performance for high-quality medical billing and coding. Save your money by outsourcing to a professional billing service.

